The conversation about mental health often centers on the two most common categories of disorders: Anxiety Disorders and Depressive Disorders. Globally and within the United States, these two categories consistently rank as the most prevalent, impacting hundreds of millions of people and representing the largest burden of disease in terms of lost productivity and disability.
Determining the third most common mental illness is a nuanced task, as the ranking can shift slightly depending on the specific study, the methodology used (e.g., lifetime prevalence vs. 12-month prevalence), and the population surveyed (global vs. national). However, based on broad national and international data from major health organizations, after Anxiety Disorders and Depressive Disorders, the third most commonly cited mental illness in terms of overall lifetime prevalence and impact is often Substance Use Disorder (SUD) or Post-Traumatic Stress Disorder (PTSD), depending on how major categories are grouped.
Focusing on individual, clinically diagnosable conditions, and excluding the broader categories of Anxiety and Depression, the next significant challenges often include Post-Traumatic Stress Disorder (PTSD) or the overarching category of Substance Use Disorders (including alcohol and drug use disorders). Given the pervasive nature of trauma and the co-occurring link between mental illness and substance use, both deserve examination.
Post-Traumatic Stress Disorder (PTSD): The Third Tier Challenge
Post-Traumatic Stress Disorder (PTSD) is often cited as one of the most common disorders after the two leading categories, especially when looking at adult lifetime prevalence. PTSD is a condition that develops in some people who have experienced a shocking, terrifying, or dangerous event.
Why PTSD is a Major Issue:
- Intrusive Symptoms: The core of PTSD involves experiencing the trauma again through flashbacks, nightmares, and intrusive thoughts. These symptoms are emotionally and physically exhausting, hijacking the individual’s present moment and disrupting normal functioning.
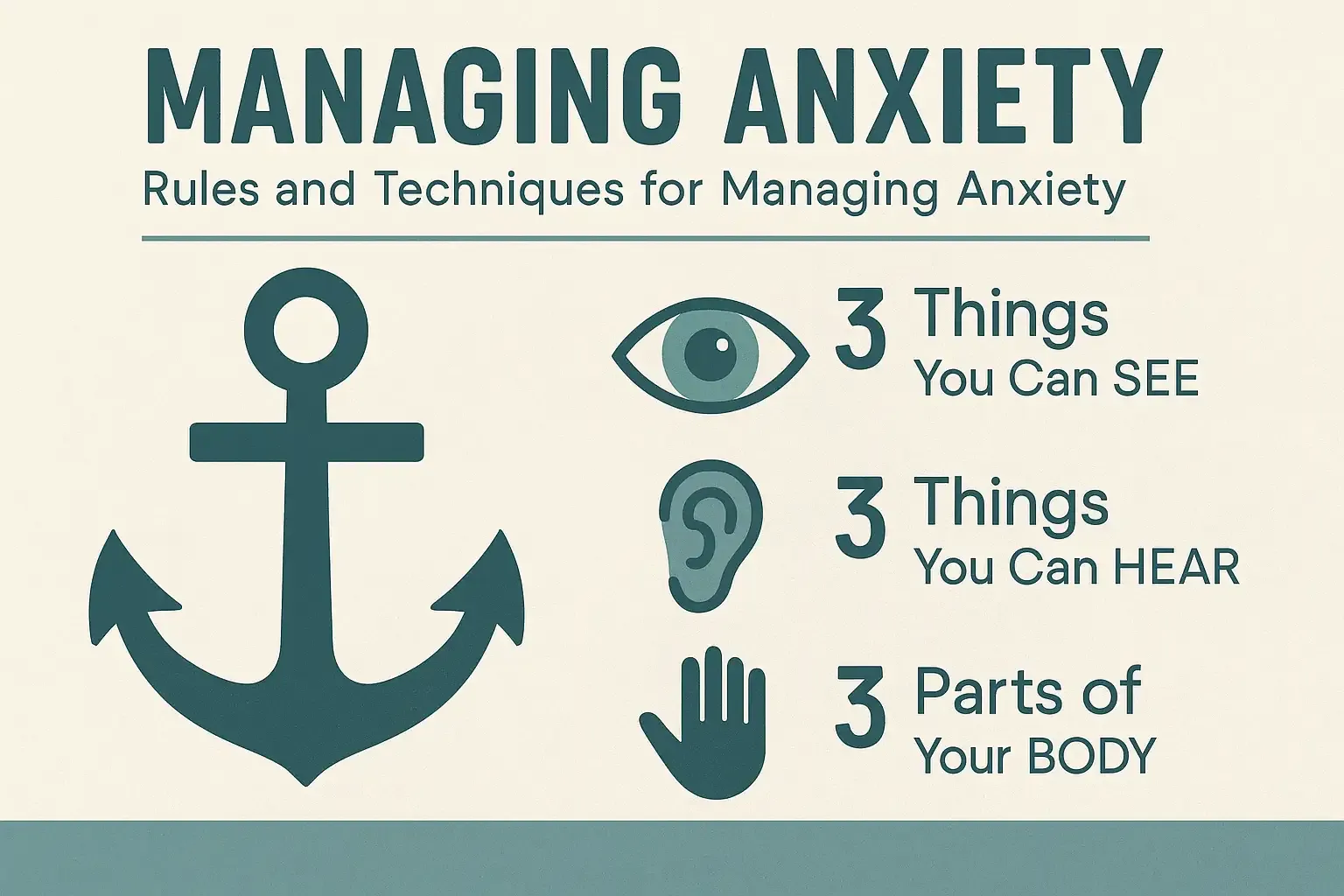
- Avoidance and Hyperarousal: People with PTSD actively avoid places, people, or activities that remind them of the trauma, leading to significant social and occupational impairment. This is coupled with a state of chronic hyperarousal—being constantly on edge, easily startled, and experiencing difficulty sleeping and concentrating.
- Comorbidity: PTSD rarely exists in isolation. It frequently co-occurs with Anxiety Disorders, Major Depressive Disorder, and Substance Use Disorder as individuals attempt to self-medicate or numb the painful intrusive symptoms.
The clinical focus for PTSD is on therapeutic and pharmacological options. Trauma-focused therapies, such as Eye Movement Desensitization and Reprocessing (EMDR) and Cognitive Processing Therapy (CPT), are highly specialized and effective clinical treatments designed to help the brain process and integrate the traumatic memory so it no longer causes a constant state of threat.
The Pervasiveness of Substance Use Disorders (SUD)
When mental health prevalence is discussed, Substance Use Disorders (SUD) must be included, as they are intrinsically linked to other mental health conditions and represent a massive community burden. Often, substance use begins as a maladaptive coping mechanism for underlying and untreated anxiety or depression.
The Role of SUD in the Mental Health Picture:
- Self-Medication: A significant number of individuals with mental health challenges turn to alcohol or drugs to temporarily quiet intrusive thoughts, dampen overwhelming anxiety, or lift depressive moods. Over time, this reliance escalates into a clinical disorder.
- Complex Treatment: The presence of both a mental illness and a substance use disorder (co-occurring disorders) requires an integrated, interdisciplinary treatment approach. It is not possible to effectively treat one without simultaneously addressing the other.
The Community Perspective and Clinical Response
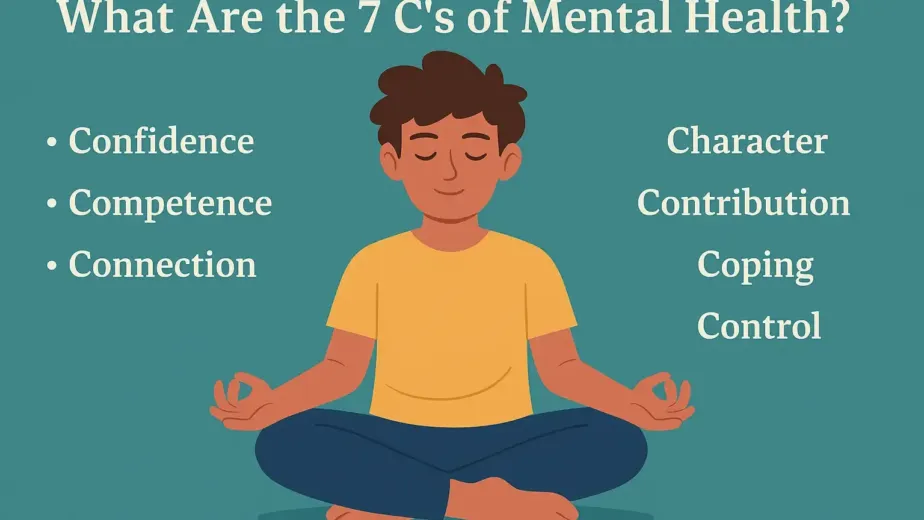
The ranking of the third most common disorder underscores a fundamental principle: a significant percentage of our community is struggling with severe, chronic mental health challenges that go beyond simple sadness or stress. Whether it is PTSD, SUD, or other conditions like Bipolar Disorder or Obsessive-Compulsive Disorder (OCD) which also rank high in terms of impact, the message is clear.
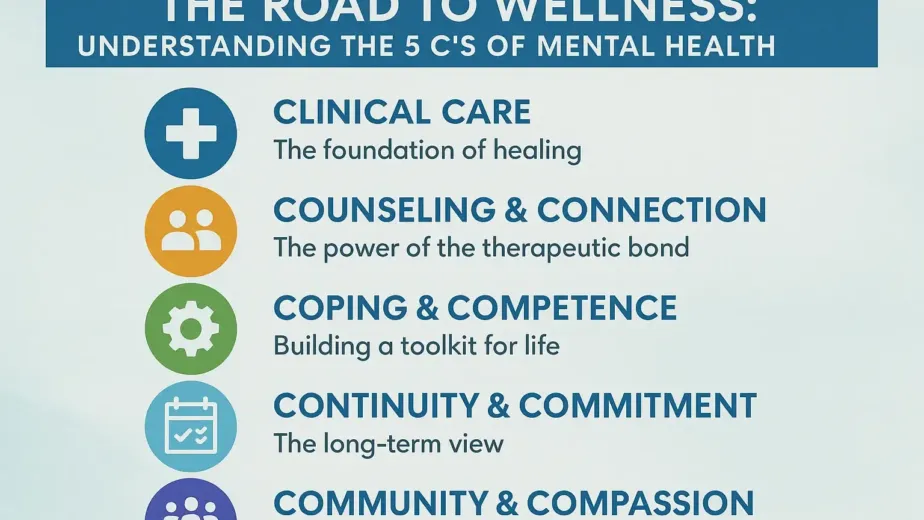
These prevalent illnesses require access to comprehensive, professional clinical care. This includes:
- Integrated Care: Providing a treatment model that can address psychiatric needs (medication management), therapeutic needs (counseling and specialized trauma therapy), and, where necessary, substance use treatment (IOP or PHP services).
- Accessibility: Ensuring that care is available and accessible across the community, regardless of a person’s ability to pay, through accepting a wide range of private and public insurances.
Understanding the prevalence of these conditions should dissolve the remaining stigma and galvanize the community to support and utilize the clinical resources available for recovery.