In our community, we often talk about physical fitness—going to the gym, eating well, getting rest—but mental fitness is just as critical. Behavioral health isn’t simply the absence of illness; it is a trainable capacity for resilience and well-being. Promoting positive behavioral health requires focusing not just on individual coping skills, but also on supportive environments where we live and work.
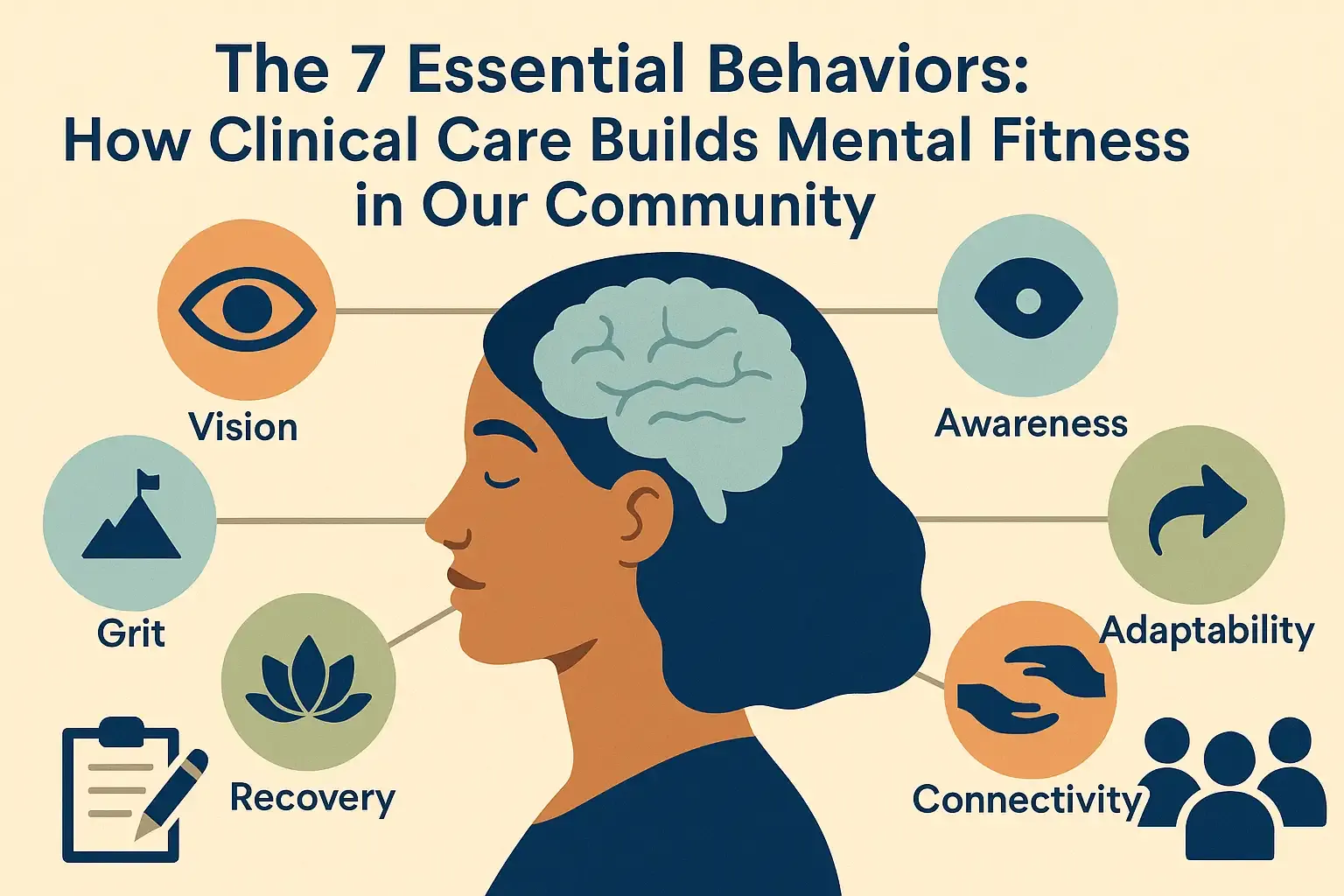
The evidence-based model of mental fitness identifies seven interdependent behaviors, or “Pillars,” that are essential for long-term psychological strength. These are: Vision, Attitude, Awareness, Adaptability, Grit, Recovery, and Connectivity.
While foundational habits like good sleep and regular exercise are protective, mastering these deeper seven behaviors often requires dedicated, professional guidance. Clinical options, including both specialized therapy and expert medication management, provide the structure and science needed to systematically train these skills and build lasting resilience.
Building a Foundation: Vision and Grit through Action
Mental fitness begins with knowing where you are going (Vision) and having the perseverance to get there (Grit).
Vision is the ability to align your daily actions with your future goals and purpose. Many people start therapy feeling unsure or overwhelmed. Clinicians address this through structured therapeutic goal setting, helping to clarify vague desires like “being happy” into specific, measurable, and achievable targets. This clarity transforms ambiguity into actionable direction.
The pursuit of goals requires Grit, which is perseverance toward meaningful objectives despite setbacks. Clinically, Grit is strengthened through Behavioral Activation (BA), a powerful strategy often used to treat depression. Depression often leads to isolation and avoidance; BA works by systematically decreasing avoidance and increasing engagement in meaningful activities, such as exercising, connecting with family, or completing basic self-maintenance. By helping clients restart activities aligned with their values, therapy activates motivational endurance.
Mastering the Mind: Attitude, Awareness, and Adaptability
The middle three pillars focus on how we perceive, regulate, and respond to the world around us.
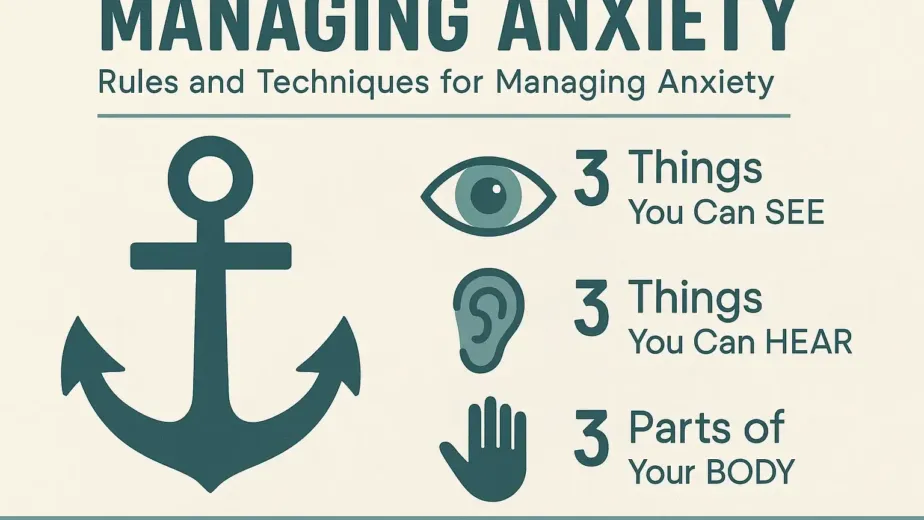
Attitude is maintaining emotional resilience under pressure. The core clinical strategy here is Cognitive Behavioral Therapy (CBT), which focuses on Cognitive Restructuring. CBT helps clients identify unhealthy, negative beliefs and challenge unhelpful thought patterns that fuel the cycle of negative feelings and behavior. Furthermore, integrating mindfulness techniques, such as mindful breathing and meditation, can positively influence cognitive biases, fostering a non-reactive, present-moment awareness.
Awareness is the skill of sensing and accurately naming internal emotional and physiological states. Without this clear sense of self, adaptive coping is impossible. Specialized modalities like Dialectical Behavior Therapy (DBT) and Acceptance and Commitment Therapy (ACT) are used to cultivate this skill. DBT provides explicit skills for emotional regulation, while ACT encourages the acceptance of difficult feelings rather than attempting to avoid them, reducing secondary distress.
Adaptability is the cognitive and emotional flexibility required to recalibrate strategies when things change. Therapy fosters this through Psychological Flexibility, helping clients remain present and act based on their values, even amidst internal discomfort. Therapists use techniques like role-playing and behavioral experiments to encourage flexible thinking, which is critical for resilience and long-term health.
Connection and Restoration: Recovery and Connectivity
The final two pillars ensure the system is rested and supported.
Recovery is the ability to restore balance and refill emotional reserves, focusing on nervous system restoration. Clinically guided relaxation is key. Therapists teach scientifically validated techniques like Progressive Muscle Relaxation (PMR), where muscle groups are systematically tensed and relaxed, and Biofeedback, which uses electronic devices to help clients learn to control body functions like heart rate and muscle tension.
Connectivity involves building strong social connections and supportive relationships. Therapy addresses this through social skills training—including assertiveness and active listening—to help clients improve communication and set boundaries. Crucially, the collaborative, trusting relationship between the client and the therapist, known as the Therapeutic Alliance, serves as a safe blueprint for external relationships. By successfully navigating conflict within this alliance, clients learn essential skills for managing disagreements and building trust outside of therapy.
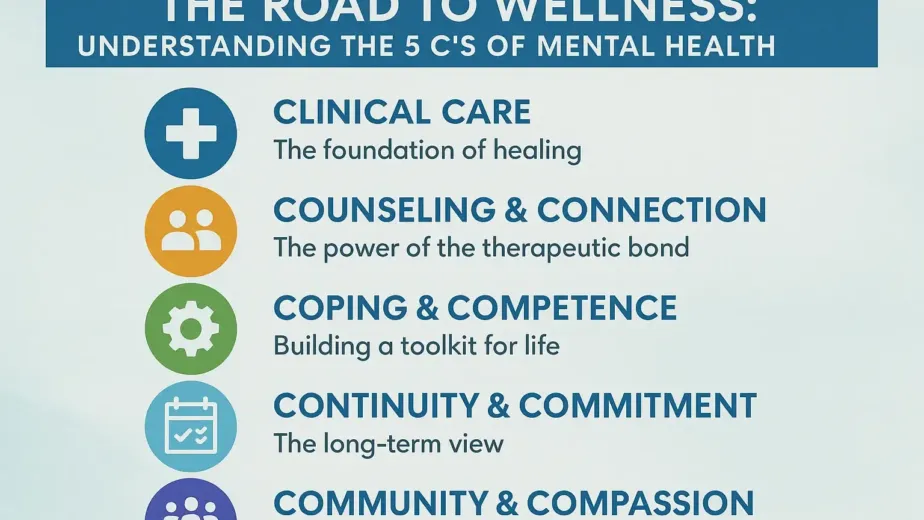
The Integrated Path: Psychotherapy and Medication
Mastering these behaviors is often accelerated through the additive model—combining psychotherapy and pharmacotherapy.
Medication works as a complementary, bottom-up approach by addressing chemical imbalances in the brain. Neurotransmitters like serotonin and dopamine, which regulate mood and behavior, are influenced by medication to restore balance and alleviate symptoms. For trauma survivors, medication can be vital in regulating the brain’s overactive alarm system (the amygdala).
This stability is essential because symptom relief from medication makes it easier for individuals to function and fully engage in therapy to build skills. Research even suggests that some antidepressants can increase the brain’s plasticity, making it more receptive to learning during cognitive and behavioral skill training. This integrated approach ensures the best chance for lasting recovery and significantly reduces the risk of relapse.
Serving Our Maryland Community
Facilities like Maryland Health Services (MDBH) are committed to this integrated model of “uncompromising excellence in mental Health Care,” providing both individualized psychotherapy and expert medication management. By offering holistic solutions, MDBH helps to overcome critical barriers like stigma and lack of access. As a mission-driven organization, MDBH provides services tailored for Medicaid participants in Maryland, ensuring comprehensive coverage for outpatient therapy, crisis intervention, and substance use disorder treatment.
Seeking support is a commitment to specialized training. By acknowledging the need for a professional guide and embracing the integrated path, you begin the active process of developing your innate capacity for robust mental fitness. Resources like the Substance Abuse and Mental Health Services Administration (SAMHSA) can also help anonymously locate treatment options across the U.S..